Thermal processing of carbohydrates reduces their glycemic index
Why one should consider cooling and re-heating of carbs
According to the World Health Organisation “diabetes has entered the top 10 causes of death, following a significant percentage increase of 70% since 2000. Diabetes is also responsible for the largest rise in male deaths among the top 10, with an 80% increase since 2000”.
Type 2 diabetes is mostly man made, therefore preventable
Considering that type 2 diabetes is preventable, man made and caused by our dietary habits, it is a matter to be taken seriously. It’s also a fairly new disease, connected direcetly to the modern diet. Our ancestors from a few generations ago didn’t get diabetes as they ate differently. As researchers from Berkeley put it “the modern diabetes epidemic is caused, not by a virulent pathogen, but by the spread of an even stealthier invader: the Western lifestyle”.
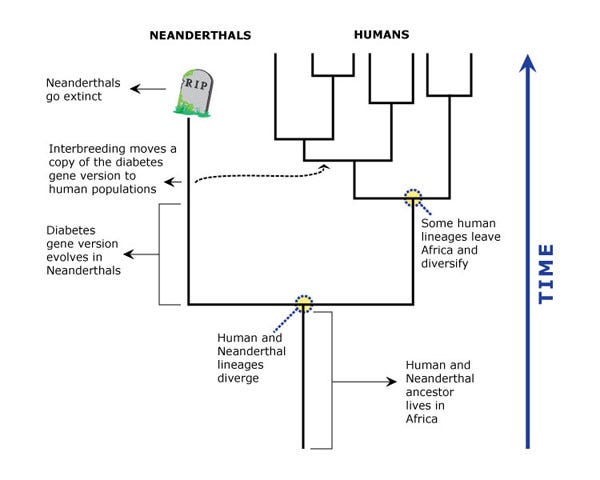
There are also, as it turns out, genetic factors that increase chances of developing the disease. Due to this gene, Mexicans and Latin Americans, for example, have nearly twice the chance of developing diabetes that non-Hispanic white Americans do. Because it takes genes a lot (thousands and hundreds of thousands of years) of time to evolve and mutate, it has been hypothethise that this mutation must have started around 800,000 years ago, meaning that perhaps the diabetes-contributing gene didn't actually evolve in our direct ancestral lineage, but in Neanderthals.
This doesn’t mean that Neanderthals had diabetes. “Type 2 diabetes is a disease of the modern world, borne of a mismatch between modern, unhealthy lifestyles and a metabolism that, for the vast majority of our evolutionary history, existed in an environment where food was relatively scarce and lots of physical activity was necessary to survive. In that harsh environment, even individuals carrying genes that contribute to diabetes when food is plentiful and sedentary lifestyles are common are unlikely to develop diabetes”.
There are many ways to prevent type 2 diabetes with eTRF (early time-restricted feeding) as one of the most effective ones. But this is a topic for a separate post so I’ll leave it at this point. Let’s take a look at the diabetes phenomenon from a different angle. As study shows, rodents don’t develop diabetes in their natural habitat or if fed with the food dedicated to them. However, if only rodents get too much of human food, they get all sorts of diseases including diabetes.
Starch vs. resistant starch
If you are not on a ketogenic diet, you are most probably eating lots of carbs daily. Pasta, potatoes, bread and rice are all carbohydrates that cause a surge in blood glucose levels as they are broken down. For people with diabetes, these surges in glucose can be leathal at worst and tricky to manage, causing severe problems over time at best.
Starch is the most common carbohydrate in our diets and is essentially a chain of glucose molecules linked together. Raw starchy foods (e.g. raw potatoes) have a highly ordered structure and are hard to digest, but heating them in water weakens this structure, making it easier for the gut to break down each chain and absorb glucose into the blood. The not-so-magical way to decrease the glycemic index of those carbohydates is, scientifically speaking, by turning starch into resistant starch. Resistant starch is a carbohydrate that resist digestion in the small intestine and ferments in the large intestine. As the fibers ferment they act as a prebiotic and feed the good bacteria in the gut.
”When starches are digested they typically break down into glucose. Because resistant starch is not digested in the small intestine, it doesn’t raise glucose. Gut health is improved as fermentation in the large intestine makes more good bacteria and less bad bacteria in the gut. Healthy gut bacteria can improve glycemic control”.
How to make resistant starch
Here comes the easiest part. It’s super easy to make resistant starch from starch. It just takes time. As study showes, you get less glycemic index through thermal processing of carbohydrates. If you cook rice and then chill it overnight, it will have dicreased glycemic index. If you then reheat it again, it will cause the lowest rise in blood glucose.

This is a fairly new idea. “The influence of cooling we’ve known about for 20 years, but the influence of reheating after cooling was unexpected. We’re still not sure exactly why it works. All we can assume is that the process of heating, cooling and reheating pasta or other starchy foods must be creating more resistant starch.” - Says Dr Denise Robertson, senior nutrition scientist at the University of Surrey.
Actually, keeping food in low temperature (-20ºC ) alone is enough to turn starch into resistant starch, as a study from 2004 shows. “Significant increase on the RS content was evidenced for all the stored foods. The food storage resulted in a significant decrease on the GI of beans and chick-peas”. However, “the GI of pasta remained the same and the GI of corn meal increased. Thus, the RS formation showed reduced influence on the glycemic index. The storage of starchy foods under low temperature can collaborate to the RS intake but its effect on the GI will depend on the characteristics of the carbohydrates of each food”. This is were re-heating plays its part.
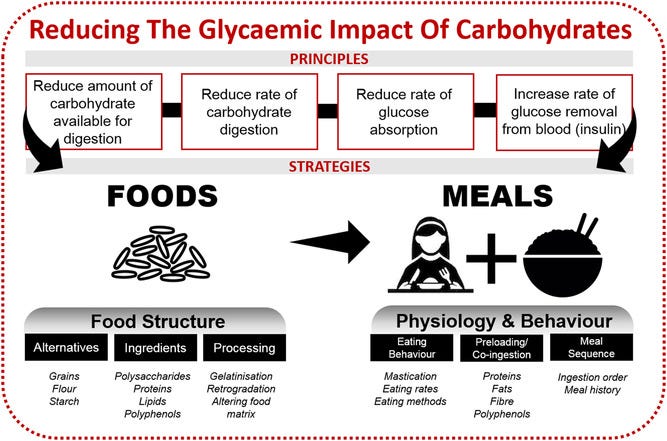
Studies have shown that consumption of cooled rice after cooking (whether reheated or not) results in lower postprandial blood glucose responses compared to freshly cooked rice (Lu, Venn, Lu, Monro, & Rush, 2017; Sonia, Witjaksono, & Ridwan, 2015), and similar effects were seen for potatoes (Tahvonen, Hietanen, Sihvonen, & Salminen, 2006). Without using alternative ingredients or adding other ingredients, it is possible to manipulate the structure of the food matrix and its subsequent digestibility via processing methods and conditions.
Conclusion
There is no one‐size‐fits‐all strategy for all foods and consumers since we differ in our metabolism, habits, allergies and many other factors. As the summary of this research paper goes, one “can try to incorporate aternative low‐GI grains such as sorghum into the diet, add alginate to rice dough formulations, cool and reheat rice prior to consumption, or consume proteins together with carbohydrates in a mixed meal to reduce starch digestibility and/or glycemic response”.